Medicare Advantage Prior Authorization Survey (2021)
Access to Inpatient Rehabilitation for Medicare Advantage Beneficiaries
An Examination of Prior Authorization Practices (2021)
Advocacy Quick Links
Abstract
The use of prior authorization (PA) by Medicare Advantage (MA) plans is a pressing concern among rehabilitation providers. A nationwide survey of rehabilitation hospitals and units (RHUs) was conducted to determine how frequently PA was used to deny admission to an RHU, how timely those decisions were rendered, and the resulting consequences for patients. The survey, which tracked data for one month (August 2021), found that MA plans overrule rehabilitation physician judgment at a rate of 53%. In addition, patients wait on average more than two and half days for a determination. This resulted in more than 30,000 days waiting for determinations during the single survey month. Since the vast majority of patients being referred to an RHU are hospitalized in an acute hospital, enormous cost and burden results from the use of PA. In addition, seriously impaired MA beneficiaries may be harmed by denials and delays in access to care.
Online Courses
You’ve come to the right place for exceptional learning opportunities from leaders in the medical rehabilitation industry. AMRPA webinars offer insights and best practices from the comfort of your desk.
Introduction and Background
Medicare Advantage (MA) plans offer different premiums and cost-sharing options than traditional Medicare (TM) and include additional health and wellness benefits. They can also use strategies like prior authorization (PA) for payments. Despite these differences, MA plans must still provide all benefits available in TM.
Enrollment in MA plans has rapidly increased, with around 28 million of the 64 million Medicare beneficiaries now using them. However, providers report that PA determinations and denials have increased, often not following evidence-based guidelines, causing care delays and negative clinical outcomes. There’s also concern over the lack of accountability and data transparency regarding PA use.
In rehabilitation hospitals and units (RHUs), PA can delay patient discharge from acute hospitals and access to needed therapies. RHUs, or Inpatient Rehabilitation Facilities (IRFs), offer intensive, physician-directed care aimed at improving patients’ functional capacities. Medicare requires that a rehabilitation physician approves each admission and that patients benefit from intensive therapy. RHUs treat more seriously ill patients than other post-acute settings.
Medicare does not have specific PA response time regulations for hospitalized patients, leading to increased burden and high denial rates for PA requests. There’s limited publicly available data on PA outcomes at the initial determination or appeal levels. The American Medical Rehabilitation Providers Association (AMRPA) conducted a survey to gather more information on PA use, denial frequencies, and care delays in RHUs.
Certification
The AMRPA certification program is designed to support new leaders and promote consistency and professionalism in rehabilitation management.
Survey Objectives
The goals of this survey were to determine how common denials of authorization for RHU care are, how timely those determinations are made, and what the consequences of those determinations may be.
Design
RHUs were solicited to participate prospectively in a data collection effort for the month of August 2021. The survey was publicized through trade association and professional channels to the RHU community, including disclosure of the specific questions that would be included on the survey and a spreadsheet form that could be used to capture the PA activity as it occurred. Participants submitted their data via an online portal.
The survey consisted of nine questions, shown in Table 1.
Participants
Data were submitted by 102 respondents who provided information about a total of 475 RHUs, representing approximately 40% of the RHUs nationwide. The responses included RHUs from 47 states and Puerto Rico. Data on 12,157 PA requests for the month of August 2021 were included in the survey.
Results
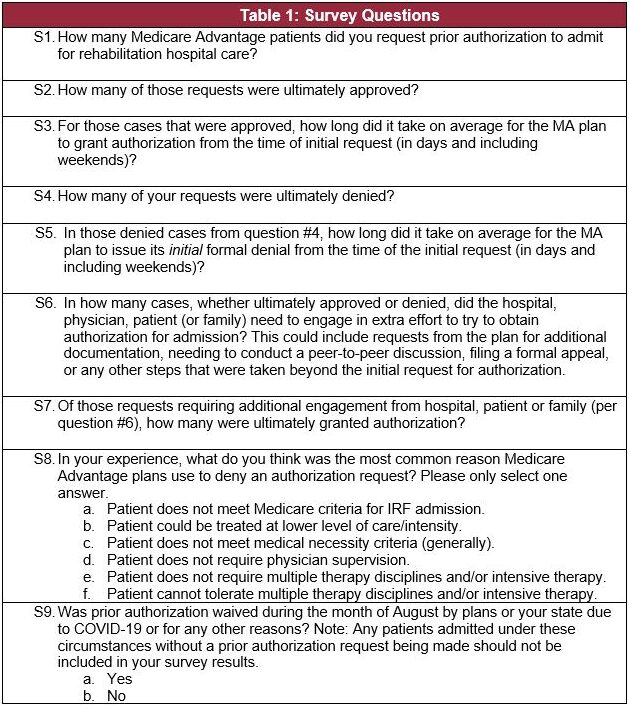
Of the 12,157 PA requests reported for the month, 6,482 of those requests were initially denied by the MA plan (53.32% of all requests). 84% of respondents reported that 30-70% of initial requests were denied during the survey month. Figure 1 shows the distribution of denial frequency cited by RHUs.
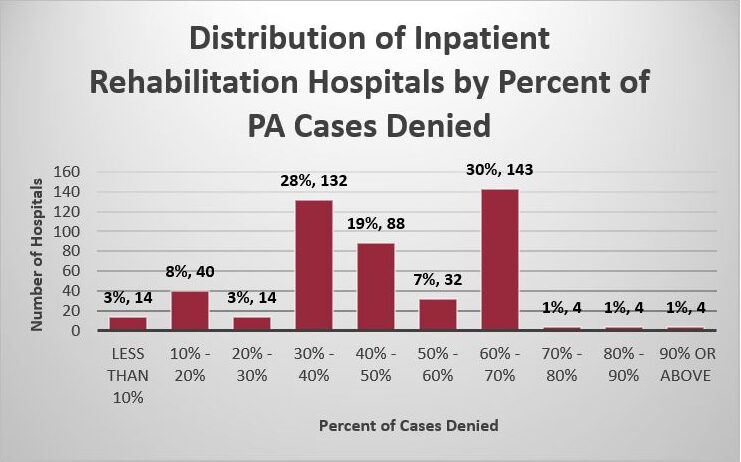
Figure 1. Distribution of Hospitals by denials
Wait times of greater than 2 days for requests were typical for the vast majority of respondents, with 84% of respondents waiting more than 2 days on average for all requests. The average wait time for the initially approved requests was 2.49 days. The average wait time for the initially denied requests was 2.59 days.
The wait times were very consistent across all IRFs. 84% of RHUs also reported an average wait time of 2.1 days or greater for denied requests. For approved requests, the majority (56%) had wait periods over two days. Figure 2 shows the distribution of wait time for a negative response. Figure 3 shows delays experienced when an initial favorable response was received.
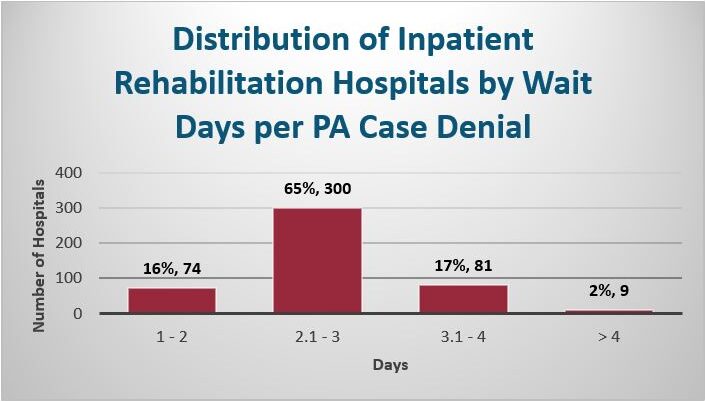
Figure 2. Distribution of Hospitals by wait time for negative response
A total of 14,152 acute hospital days were spent waiting for requests that were ultimately approved, and 16,774 acute hospital days were spent waiting for denied requests, totaling 30,926 total acute hospital days spent waiting for a determination.
Respondents provided information regarding any additional effort required to seek authorization for 4,823 requests. 35.39% of these requests required additional effort on behalf of the hospital, physician, patient or family. For requests that required this additional effort, 28.94% were approved for admission as part of the initial request.
The most commonly provided reason for a denial cited by RHUs was that the patient “could be treated at a lower level of care/intensity.” The next most common reason was that the patient “does not meet medical necessity criteria.” Some respondents indicated multiple rationales for denying payment so the total of reasons reported exceeds 100%. Finally, 29% (136) of respondents indicated that PA was waived at some point during the survey month by plans or regulators due to the COVID-19 pandemic.
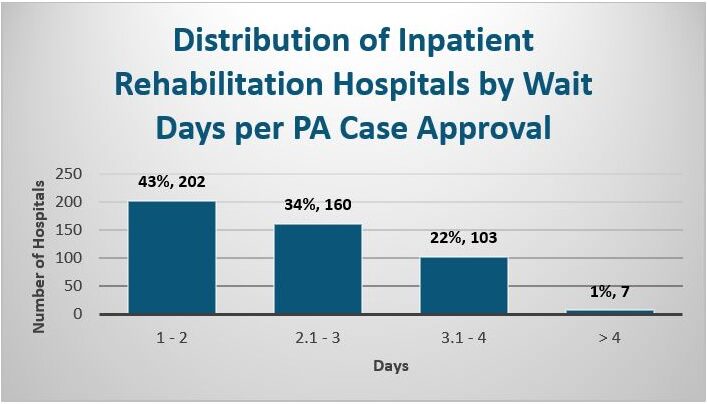
Figure 3. Distribution of Hospitals by wait time for favorable response
Certification
The AMRPA certification program is designed to support new leaders and promote consistency and professionalism in rehabilitation management.
Discussion
Prior authorization (PA) is frequently used to deny patient access to rehabilitation hospital units (RHUs), making appeals challenging due to time constraints for patient transfer. Even when MA plans approve requests, significant delays in communication occur, posing a risk to patient health. The high denial rate indicates a disconnect between rehabilitation physicians’ medical decisions and MA plans’ judgments, raising concerns about the criteria and expertise used by the plans.
MA plans often deny requests, claiming patients could be treated in lower-intensity settings, contrary to Medicare guidelines. This practice conflicts with Medicare standards, which focus on whether patients meet specific criteria for RHU admission. These findings align with other surveys indicating improper guidelines used by MA plans.
Patients in traditional Medicare (TM) would likely have been admitted to RHUs without delay. However, those in MA plans face denials due to opaque review processes. MA plans are required to issue determinations within 72 hours, but delays often extend beyond this, adversely affecting patient recovery and clinical outcomes.
This data, collected during the COVID-19 pandemic, highlights the risks and costs associated with delayed transfers. Since MA plans pay for hospital admissions prospectively, hospitals bear immediate additional costs, which can lead to increased Medicare payments due to extended patient stays.
Conclusions
MA plans’ use of the PA process to delay and deny patient transfers of from acute hospitals to RHUs is a widespread and common problem that can harm patients. PA processes increase administrative burden, delay necessary care, and increase waste and cost to the health care system.
There is an urgent need to eliminate these unnecessary delays in providing care to patients and mitigate denials based on opaque and inconsistent criteria. These needs can be addressed by regulatory and contractual changes to the MA plan operational requirements, and by ensuring that qualified clinicians are making proper and timely determinations about RHU referrals.
References
- 42 C.F.R. § 422.101.
- Bob Herman, Medicare Advantage enrollment soars almost 9%, Axios (Jan. 18, 2022), https://www.axios.com/medicare-advantage-enrollment-2022-soars-055b6d7d-d2c7-4e69-9eba-420c0ee4ef6e.html.
- American Medical Association, 2020 AMA Prior Authorization (PA) Physician Survey, (April, 2021) https://www.ama-assn.org/system/files/2021-04/prior-authorization-survey.pdf & https://www.ama-assn.org/system/files/2021-05/prior-authorization-reform-progress-update.pdf.
- American Medical Association, 2021 AMA Prior Authorization (PA) Physician Survey, (February, 2022) https://www.ama-assn.org/system/files/prior-authorization-survey.pdf
- HHS Office of Inspector General (OIG), Medicare Advantage Appeal Outcomes and Audit Findings Raise Concerns About Service and Payment Denials (Sept. 25, 2018) (https://oig.hhs.gov/oei/reports/oei-09-16-00410.asp).
- 42 C.F.R. 412.622.
- CMS Inpatient Rehabilitation Facility Data, General Information Data Set (December 2021), https://data.cms.gov/provider-data/topics/inpatient-rehabilitation-facilities.
- Assessment of Patient Outcomes of Rehabilitative Care Provided in Inpatient Rehabilitation Facilities (IRFs) and After Discharge; Dobson & Davanzo (July 2014) (https://amrpa.org/wp-content/uploads/2025/03/Dobson-DaVanzo-Final-Report-Patient-Outcomes-of-IRF-v.-SNF.pdf)
- CMS IRF PPS Coverage Requirements Nov. 12, 2009 National Provider Conference Call (“Notice that nowhere on the slide and nowhere in this presentation are we going to talk about whether the patient could have been treated in a skilled nursing facility or another setting of care. Under the new requirements, a patient meeting all of their required criteria for admission to an IRF would be appropriate for IRF care whether or not he or she could have been treated in a skilled nursing facility.”).
- American Medical Association, 2020 AMA Prior Authorization (PA) Physician Survey, (April, 2021) https://www.ama-assn.org/system/files/2021-04/prior-authorization-survey.pdf & https://www.ama-assn.org/system/files/2021-05/prior-authorization-reform-progress-update.pdf.
- 42 C.F.R. § 422.572(a).
- American Medical Association, 2020 AMA Prior Authorization (PA) Physician Survey, (April, 2021) https://www.ama-assn.org/system/files/2021-04/prior-authorization-survey.pdf & https://www.ama-assn.org/system/files/2021-05/prior-authorization-reform-progress-update.pdf.
- Why Medicare Advantage Plans Pay Hospitals Traditional Medicare Prices, Robert A. Berenson, Jonathan H. Sunshine, David Helms, and Emily Lawton, Health Affairs 2015 34:8, 1289-1295 (https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.1427).

