Medicare Advantage Prior Authorization Survey
Access to Inpatient Rehabilitation for Medicare Advantage Beneficiaries
An Examination of Prior Authorization Practices (2024)
Advocacy Quick Links
Abstract
The use of prior authorization by Medicare Advantage (MA) plans has long been a pressing concern among patients and inpatient rehabilitation providers. A nationwide survey of freestanding inpatient rehabilitation hospitals and rehabilitation units of acute care hospitals (collectively known as IRFs) was conducted to determine how frequently prior authorization for admission to an IRF was denied, how timely those decisions were rendered, and the resulting consequences for patients. The survey, which tracked data across two months (July-August 2024), found that MA plans typically overrule rehabilitation physician judgment by denying admissions at a rate of more than 57%. While new regulatory reforms that were intended to improve MA prior authorization practices went into effect in January 2024, the rate is even higher than identified in a previous survey conducted in August 2021. (1)
In 2024, these denials resulted in more than 67,000 days waiting for determinations across those two months. Since the vast majority of patients being referred to an IRF are hospitalized in an acute care hospital, the days spent awaiting an eventual approval of admission result in significant cost and burden to the health care system. Moreover, seriously impaired MA beneficiaries in need of intensive rehabilitation are harmed by denials and delays in access to care.
See below for AMRPA’s full survey results and contact AMRPA staff with any questions.
Introduction and Background
Use of Prior Authorization in the Medicare Advantage Program
Medicare Advantage (MA) plans offer various premium and cost-sharing arrangements that differ from Traditional Medicare (TM, also known as Fee-for-Service Medicare), as well as health and wellness benefits not offered to beneficiaries enrolled in TM. In addition to financial flexibilities, MA plans are permitted to employ various “utilization management” strategies not typically available in TM, including requiring prior authorization of an item or service as a condition of payment. When prior authorization is required by MA plans, the plan must provide the pre-approval or payment will not be made to the provider. While the use of prior authorization to manage benefits is permitted, MA plans are nonetheless obligated by law to provide all of the benefits offered in TM. (2)
The number of beneficiaries enrolled in MA plans has grown at an accelerated pace in recent years. In 2024, approximately 54% of beneficiaries enrolled in both Medicare Parts A and B (32.8 million) were enrolled in Medicare Advantage plans, the highest proportion since the program was implemented (for context, the rate was 39% five years prior in 2019). (3) As enrollment in MA has grown, providers have reported that delays in receiving prior authorization determinations and subsequent denials, across a wide range of covered items and services, have steadily increased and often do not follow appropriate evidence-based guidelines. (4) In addition, physicians consistently report that prior authorization processes often delay care and negatively impact clinical outcomes. (5) Concerns have also been raised about the lack of accountability for the use of prior authorization by MA plans, especially due to high rates of denials overturned upon appeal and insufficient publicly reported data. (6) A recent governmental watchdog report specifically found that inpatient rehabilitation services were among the “most prominent” service types that MA plans frequently denied despite claims meeting Medicare coverage rules. (7) Based on these findings, an oversight report specifically focused on MA coverage denials for post-acute care is expected in 2026. (8)
Impact of Prior Authorization on Inpatient Rehabilitation Providers
Inpatient rehabilitation hospitals and units (IRFs) are licensed hospitals that provide specialized and physician–directed care that includes close medical management and an intensive, interdisciplinary program of rehabilitation. The goals of care in an IRF include continuing medical management of the patient’s underlying health problems and improving the patient’s functional capacity so that the patient can return to the community. The vast majority of patients referred for admission to an IRF are in an acute hospital due t o severe illness or injury, such as traumatic brain injuries or strokes, spinal cord injuries, amputations, neurological disorders, and other serious conditions.
The Medicare coverage criteria for IRF admission stipulate that payment will be made if the patient would practically benefit from and tolerate intensive, multidisciplinary therapy and requires ongoing supervision by a rehabilitation physician. The Medicare rules also require that a rehabilitation physician approve each patient for admission. Due to these stringent Medicare coverage rules and the intensity of services offered, IRFs frequently treat more seriously ill and functionally impaired patients than lower–intensity post–acute care settings. MA plans typically require prior authorization for all or nearly all admissions to an IRF, which has made inappropriate prior authorization utilization a critical issue for inpatient rehabilitation providers. Prior authorization frequently and unnecessarily delays the discharge of patients from an acute care hospital following a severe injury or illness, and ultimately forestalls or denies access to needed rehabilitation care.
Medicare Advantage does not currently have regulatory requirements for prior authorization response times that are specific to hospitalized patients; instead, nearly all covered items and services are subject to a 14 calendar day response time for “standard” determinations (shortening to 7 calendar days beginning in 2026) and 72 hours for “expedited” requests. (9) This has increasingly caused concern among IRF providers given the process burden and high rates of denials while patients are in urgent need of timely rehabilitation care. In addition, there is limited publicly available data to determine the consequences of prior authorization requirements at the initial determination or first appeal level. (10) Medicare and its contractors do report the outcomes of the second level of appeal (formally referred to as “Reconsideration by an Independent Review Entity” or IRE). However, this level of appeal is rarely utilized for patients seeking admission to an IRF given the lengthy and time-consuming process, and the near-total alignment between MA plans and the “independent” entity. (11)
Recently Implemented Prior Authorization-Focused Regulations & Early Impacts
Recently, the Centers for Medicare and Medicaid Services (CMS) implemented a wide range of new restrictions on the use of prior authorization by MA plans, which included specific references to inpatient rehabilitation care. (12) These included, among others, restrictions on plans’ use of proprietary guidelines or internal (non-Medicare) coverage criteria to make prior authorization decisions, new standards for the experience and training required for plan reviewers who deny prior authorization, and more.
Despite the scope of these rules, which went into effect on January 1, 2024, IRF providers widely reported no change or even increases in the rates of denials of IRF admission for MA beneficiaries.
Given the intended effect of the 2024 regulations, and the general lack of available and accessible data on prior authorization practices and outcomes, the American Medical Rehabilitation Providers Association (AMRPA) conducted a survey of IRFs across the nation to gain more quantitative and qualitative information, including the pervasiveness of prior authorization use as a utilization management practice, frequency of denials, and associated delays in care.
Survey Objectives
The goals of this survey were to determine how common denials of prior authorization for IRF care are across the nation and by various large insurers, how timely determinations are made, and what the consequences of those determinations may be, particularly after the implementation of regulatory reforms intended to address the overuse of prior authorization.
Design
Freestanding inpatient rehabilitation hospitals and rehabilitation units of acute care hospitals were solicited to participate prospectively in a data collection effort for the months of July and August 2024. The survey was publicized through trade association and professional channels to the IRF community, including disclosure of the specific data elements that would be captured through the survey and a spreadsheet that would be used to collect prior authorization activity as it occurred and report aggregated data. Participants submitted their data via email.
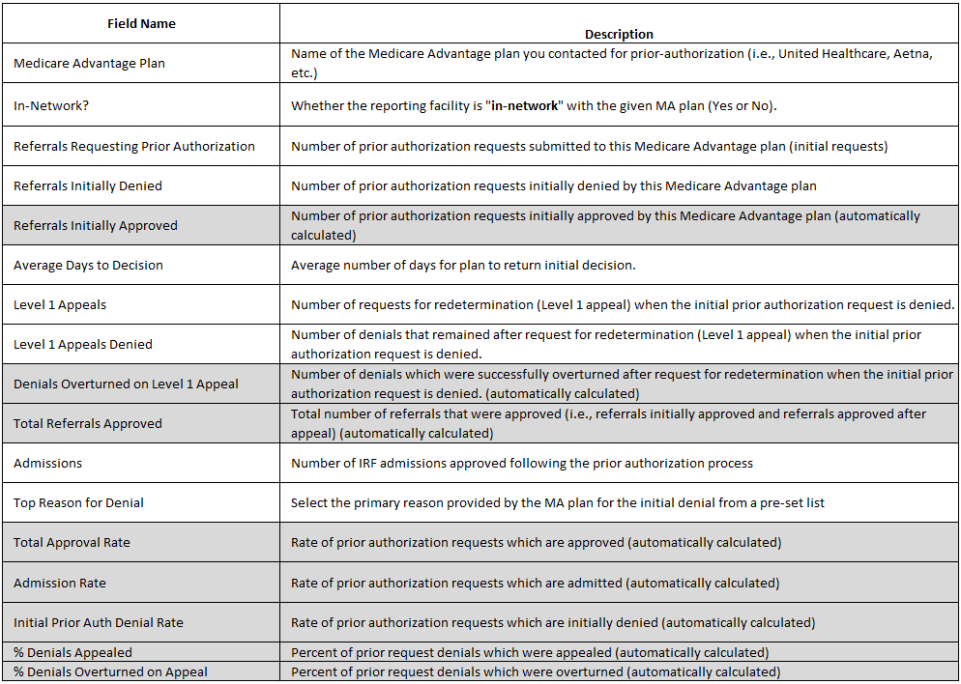
The survey tool consisted of a standardized spreadsheet in which participants submitted summary data elements for each month. Each required data element and the accompanying description are shown below in Figure 1.
Figure 1
Participants
The full data set includes responses from a total of 367 IRFs, representing approximately 30% of the IRFs nationwide. (13) The responses included IRFs from 48 states and Puerto Rico and represented nearly 19,000 licensed IRF beds. Data on a total of 27,135 requests for prior authorization (13,691 in July 2024 and 13,444 in August 2024) were reported through the survey. Of those, UnitedHealthcare accounted for 8,733 prior authorization requests (32.2%), Humana accounted for 4,954 (18.3%), and Aetna accounted for 3,803 (14%).
Results
Denials
Of the 27,135 prior authorization requests reported for the two-month period,15,571 of those requests were initially denied by the MA plan (57.4% of all requests).
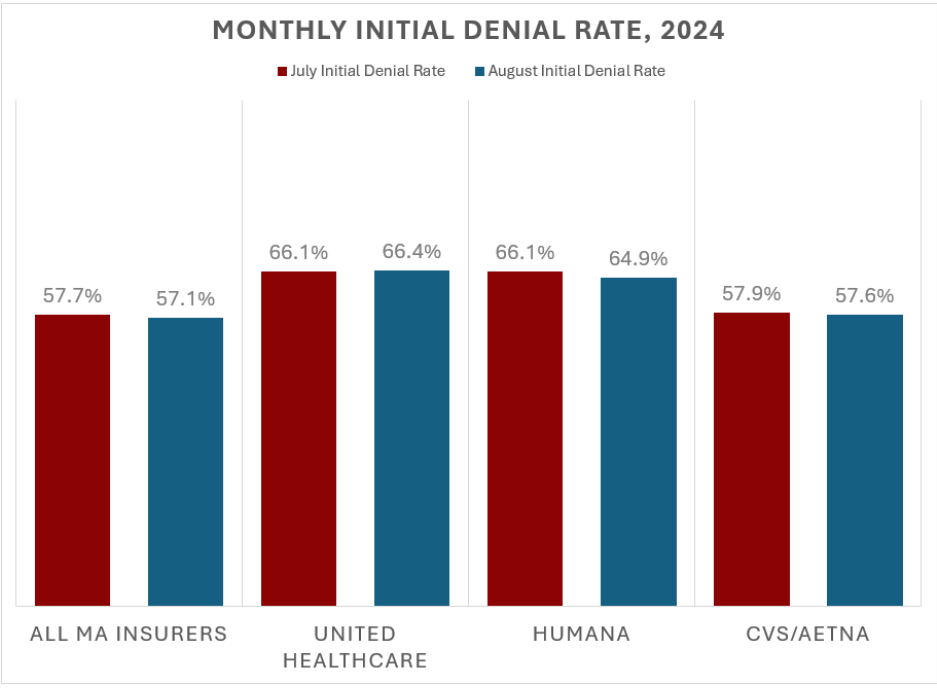
The sample’s largest MA insurers (UnitedHealthcare, Aetna, and Humana) each denied cases at a greater rate than the overall sample as well. These rates were highly stable across each month individually. UnitedHealthcare initially denied 66.3% of prior authorization requests; Humana denied 65.6%, and Aetna denied 57.7%.
Figure 2 shows the initial denial rates reported for July and August 2024.
Figure 2
Appeals
Of the more than 15,000 initial denials reported in the sample, 3,866 were appealed at “Level 1” (the plan reconsideration level). This represents an appeal rate of 24.8%.
Of those, 34.4% were overturned by the plan upon appeal (1,329). This survey did not collect information on later stages of appeal.
Admissions
IRFs in the sample reported admitting a total of 12,098 MA beneficiaries following a plan authorization during the sample period, an approximately 44.6% admission rate for those initially screened for admission into the IRF.
Some patients may have eventually been admitted outside of the sample period if the plan provided an authorization after a longer determination process, and some hospitals reported certain patients may have been transferred to another setting of care (e.g., a skilled nursing facility) before eventually receiving an authorization for IRF admission.
Timeliness
Reportable time to decision information was provided for 25,990 of the 27,135 referrals requesting prior authorization (95.8%). Across all insurers, the average wait time to an initial decision (whether approval or denial) was just over 2.5 days. (14) For the largest insurers in the sample, UnitedHealthcare’s average response time was 2.83 days and Aetna’s was 3.5; Humana provided an average response time of slightly less than the average at 2.3 days.
A total of 67,247 reported acute hospital days were spent waiting for an initial determination; additional days spent waiting while appealing an adverse decision were not collected for this survey. If the (relatively stable) rates of referrals across July and August were extrapolated for the entire calendar year, this would represent over 400,000 waiting days in 2024 just for these 367 IRFs; there are approximately 1,200 IRFs serving patients nationwide. Across the entire IRF field, prior authorization could account for as many as 1.2 million waiting days in 2024 before any initial decision is rendered.
Discussion
Prior authorization is commonly used to delay or deny patient access to IRF care. These determinations are difficult to challenge, since subsequent appeals take additional days, and patients typically are in need of more prompt treatment. Additionally, there is increasing pressure on acute care hospitals to free up beds, which can often lead to patients in need of intensive rehabilitation treatment in an IRF instead being transferred to lower-intensity settings of care, such as nursing homes or home with home health care. The data presented here show that even when an MA plan approves an initial request for authorization, there are often substantial delays in communicating that decision. With these delays and denials, there is an associated risk that patients may be harmed or their full functional recovery may be jeopardized. (15)
The high frequency of denials suggests that there is a striking disagreement between the medical decisions of practicing rehabilitation physicians and the judgments being rendered by MA plans, especially for the largest insurers in the market. Since rehabilitation physicians determined that each of these referred patients required IRF admission under the stringent Medicare coverage criteria, the widespread denials by MA plans call into question what criteria and expertise plans are relying on to render decisions, as well as the financial incentives at play in the MA program. These concerns are further heightened by reports of large MA plans using artificial intelligence, algorithms, or other automated systems to override even their own reviewers’ clinical decision-making. (16)
If any of the denied patients had been enrolled in Traditional Medicare, they likely would have been admitted to the IRF upon approval by a rehabilitation physician. Instead, because the beneficiary chose to enroll in MA, and due to the opaque review process and criteria utilized by MA plans, these patients were denied timely access to inpatient rehabilitation care. Medicare regulations require MA plans to issue determinations “as expeditiously as the enrollee’s health condition requires, but no later than 72 hours after receiving the request,” for those requests categorized as expedited by the referring provider. (17)
This survey shows that MA plans consistently do not issue determinations as expeditiously as the beneficiary’s condition requires, since such a response would be necessitated within minutes to hours, not days. It is likely that in many cases, prior authorization delays the initiation of needed therapeutic interventions and hampers patients’ recovery. This finding is again consistent with other surveys that indicate prior authorization detrimentally impacts clinical outcomes for patients. (18)
The data presented here provide only a “snapshot in time,” representing two months of activity in 2024. However, these results are not only directionally consistent with AMRPA’s prior findings from August 2021, (19) but hew closely to findings from the Medicare Payment Advisory Commission (MedPAC) that beneficiaries in Medicare Advantage typically have only one-third the access to IRF care that Traditional Medicare beneficiaries have. (20) More recently, based on MA admissions information sourced from eRehabData (21) and Netsmart Technologies Inc., UDSMR® database, MA admissions to IRF per 1,000 beneficiaries have a monthly value of between 0.35 and 0.42. For Traditional Medicare admissions and a reported 400,000 discharges per year reported by MedPAC, monthly Traditional Medicare admissions per 1,000 beneficiaries hovers around 1.0, again indicating that access to IRF care is nearly three times higher in Traditional Medicare than Medicare Advantage.
These data unfortunately also suggest that new regulatory restrictions on prior authorization have not had their intended effect on access to IRF care in MA, necessitating further emphasis from the federal government on oversight and enforcement of these rules and underscoring the need for meaningful, program-wide transparency into MA plan practices. Finally, since the vast majority of patients seeking admission to an IRF are hospitalized in an acute care hospital, each day of delay in transfer represents increased risk and cost. Because MA plans typically pay for hospital admissions on a prospective basis, the immediate additional cost is borne by the referring hospital; aside from these fiscal pressures, such practices also exacerbate bed capacity issues. (22) As these additional lengths of stay are captured through Medicare’s tracking of resource utilization, payments may be increased due to extended length of stay for these patients, costing Medicare additional unnecessary dollars.
Conclusions
Medicare Advantage plans’ use of prior authorization to delay and deny patient access to medically necessary care is a widespread and common problem. In the inpatient rehabilitation context, prior authorization processes as currently used particularly increase administrative burden, delay medically necessary care, and increase waste and cost to the health care system.
There is an urgent need to eliminate these unnecessary delays in providing care to patients and mitigate denials based on opaque and inconsistent criteria. These needs can be addressed by legislative and regulatory reforms, as well as increased oversight and enforcement of MA plan behaviors, and by returning discretion to the qualified physicians treating patients on the ground, rather than bureaucratic processes at the MA plan level.
References
1. American Medical Rehabilitation Providers Association, Access to Inpatient Rehabilitation for Medicare
Advantage Beneficiaries: An Examination of Prior Authorization Practices (2021), https://amrpa.org/medicare-advantage-prior-authorization-survey-2021/.
2. 42 C.F.R. § 422.101(b).
3. Meredith Freed, Jeannie Fuglesten Biniek, Anthony Damico, and Tricia Neuman, Medicare Advantage in 2024: Enrollment Update and Key Trends (KFF, Aug. 2024) https://www.kff.org/medicare/issuebrief/medicare-advantage-in-2024-enrollment-update-and-key-trends/.
4. American Medical Association, 2024 AMA Prior Authorization (PA) Physician Survey (February 2025),
https://www.ama-assn.org/system/files/prior-authorization-survey.pdf.
5. Id.; the AMA has collected similar surveys on an annual basis in recent years, which have yielded similar results.
6. Department of Health and Human Services (HHS) Office of Inspector General (OIG), Medicare Advantage Appeal Outcomes and Findings Raise Concerns About Service and Payment Denials (September 2018), https://oig.hhs.gov/oei/reports/oei-09-16-00410.pdf.
7. HHS OIG, Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns about Beneficiary Access to Medically Necessary Care (April 2022), https://oig.hhs.gov/oei/reports/oei-09-18-00260.pdf.
8. HHS OIG, Medicare Advantage Organizations’ Use of Prior Authorization for Post Acute Care (Expected FY 2026), https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000873.asp.
9. 42 C.F.R. §§ 422.568(b)(1), 422.572(a)(1).
10. Beginning in 2026, MA plans will be required to report certain aggregated metrics for prior authorizations, covering all items and services (see 42 C.F.R. § 156.223).
11. Piper, Jermaine and Lane Koenig, Medicare Advantage Prior Authorization Denials for Post-Acute Care Are Rarely Overturned, KNG Health Consulting (June 11, 2024). https://www.knghealth.com/medicareadvantageprior-authorization-denials-for-post-acute-care-are-rarely-overturned/. (Finding that between January 1, 2020 and March 31, 2024, Medicare’s IRE reviewed 48,938 appeals of IRF admission denials by MA organizations, and only overturned 764, while upholding more than 48,000 denials).
12. Medicare Program; Contract Year 2024 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly, 88 Fed. Reg. 22120 (April 12, 2023).
13. CMS Inpatient Rehabilitation Facility Data, General Information Data Set (December 2024), https://data.cms.gov/provider-data/topics/inpatient-rehabilitation-facilities
14. Hospitals in the sample reported an “average time to decision” for each MA plan included in their sample; the average response time was calculated by creating a total number of waiting days for each plan (average response time per plan multiplied by total referrals to that plan), producing a total number of waiting days in the sample, and dividing by the total number of referrals.
15. Assessment of Patient Outcomes of Rehabilitative Care Provided in Inpatient Rehabilitation Facilities (IRFs) and After Discharge; Dobson & Davanzo (July 2014), https://amrpa.org/wp-content/uploads/2025/03/Dobson-DaVanzo-Final-Report-Patient-Outcomes-of-IRF-v.-SNF.pdf.
16. See, e.g., Casey Ross and Bob Herman, STAT News, How UnitedHealth’s Acquisition of a Popular Medicare Advantage Algorithm Sparked Internal Dissent over Denied Care (July 11, 2023), https://www.statnews.com/2023/07/11/medicare-advantage-algorithm-navihealth-unitedhealth-insurance-coverage/.
17. 42 C.F.R. § 422.572(a)(1).
18. American Medical Association, 2023 AMA Prior Authorization (PA) Physician Survey (July 2024), https://www.ama-assn.org/system/files/prior-authorization-survey.pdf.
19. American Medical Rehabilitation Providers Association, Access to Inpatient Rehabilitation for Medicare
Advantage Beneficiaries: An Examination of Prior Authorization Practices (2021), https://amrpa.org/medicare-advantage-prior-authorization-survey-2021/.
20. Medicare Payment Advisory Commission, Report to The Congress: Medicare Payment Policy 298 (Mar. 2017), https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/mar17_entirereport224610adfa9c665e80adff00009edf9c.pdf#page=324.
21. eRehabData® is AMRPA’s outcomes and policy modeling system.
22. Why Medicare Advantage Plans Pay Hospitals Traditional Medicare Prices, Robert A. Berenson, Jonathan H. Sunshine, David Helms, and Emily Lawton, Health Affairs 2015 34:8, 1289-1295. https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.1427.

